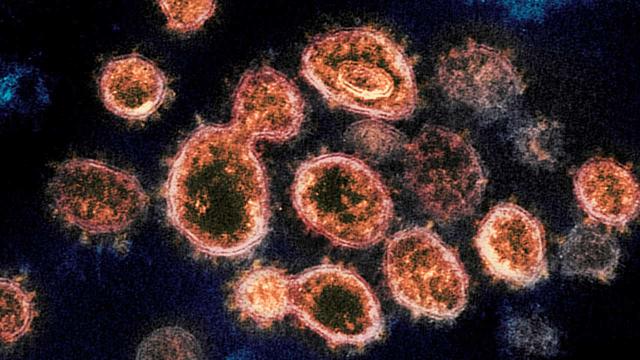
Researchers are learning that the coronavirus can infect neurons and may cause lasting damage in some cases.
Kateryna Kon/Science SourceMonths after a bout with COVID-19, many people are still struggling with memory problems, mental fog and mood changes. One reason is that the disease can cause long-term harm to the brain.
"A lot of people are suffering," says Jennifer Frontera, a neurology professor at the NYU Grossman School of Medicine.
Frontera led a study that found that more than 13% of hospitalized COVID-19 patients had developed a new neurological disorder soon after being infected.A follow-up study found that six months later, about half of the patients in that group who survived were still experiencing cognitive problems.
The current catalog of COVID-related threats to the brain includes bleeding, blood clots, inflammation, oxygen deprivation and disruption of the protective blood-brain barrier. And there's new evidence in monkeys that the virus may also directly infect and kill certain brain cells.
Studies of brain tissue suggest that COVID-related changes tend to be subtle, rather than dramatic, says Geidy Serrano, director of the laboratory of neuropathology at Banner Sun Health Research Institute. Even so, she says, "Anything that affects the brain, any minor insult, could be significant in cognition."
Shots - Health News
New clues to the biology of long COVID are starting to emerge
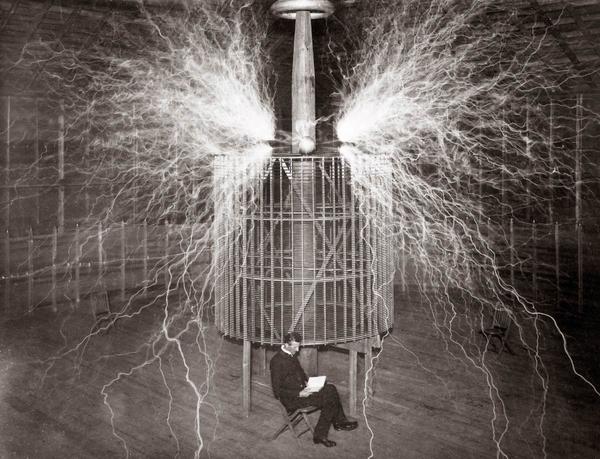
Some of the latest insights into how COVID-19 affects the brain have come from a team of scientists at the California National Primate Research Center at UC Davis.
When COVID-19 arrived in the U.S. in early 2020, the team set out to understand how the SARS-CoV-2 virus was infecting the animals' lungs and body tissues, says John Morrison, a neurology professor who directs the research center.
But Morrison suspected the virus might also be infecting an organ that hadn't yet received much attention.
"Early on, I said, 'let's take the brains,' " he says. "So we have this collection of brains from these various experiments and we've just started to look at them."
One early result of that research has generated a lot of interest among scientists.
"It's very clear in our monkey model that neurons are infected," says Morrison, who presented some of the research at the Society for Neuroscience meeting in November.
Neurons are the brain cells that make thinking possible. But studies of human brains have produced conflicting evidence on whether these cells are being infected by the virus.
The monkey brains offer an opportunity to learn more because they come from a close relative of humans and are easier to study and scientists know precisely how and when each animal brain was infected.
The monkey model isn't perfect, though. For example, COVID-19 tends to produce milder symptoms in these animals than in people.
Even so, Morrison says, scientists are likely to find infected human neurons if they look closely enough.
"We're looking at individual neurons at very high resolution," he says, "so we can see evidence of infection."
The infection was especially widespread in older monkeys with diabetes, he says, suggesting that the animals share some important COVID-19 risk factors with people.
In the monkeys, the infection appeared to start with neurons connected to the nose. But Morrison says that within a week, the virus had spread to other areas in the brain.
"This is where you get into some of the neurologic symptoms that we see in humans," he says — symptoms such as cognitive impairment, brain fog, memory issues and changes in mood. "I suspect that the virus is in the regions that mediate those behaviors."
That hasn't been confirmed in people. But other researchers have found evidence that the virus can infect human brain cells.
A draft of a study of brains from 20 people who died of COVID-19 found that four contained genetic material indicating infection in at least one of 16 areas studied.
And, similar to monkeys, the virus seemed to have entered through the nose, says Serrano, the study's lead author.
"There's a nerve that is located right on top of your nose that is called the olfactory bulb," she says. That provides a potential route for virus to get from the respiratory system to the brain, she says.
Serrano says the virus appears able to infect and kill nerve cells in the olfactory bulb, which may explain why many COVID patients lose their sense of smell — and some never regain it.
In other brain areas, though, the team found less evidence of infection.
That could mean that the virus is acting in other ways to injure these areas of the brain.
For example, studies show that the virus can infect the cells that line blood vessels, including those that travel through the brain.So when the immune system goes after these infected cells, it could inadvertently kill nearby neurons and cause neurological problems, Serrano says.
COVID-19 can also damage the brain by causing blood clots or bleeding that result in a stroke. It can damage the protective cells that create what's known as the blood-brain barrier, allowing entry to harmful substances, including viruses. And the disease can impair a person's lungs so severely that their brain is no longer getting enough oxygen.
These indirect effects appear to be a much bigger problem than any direct infection of neurons, Frontera says.
"People have seen the virus inside of brain tissue," she says. "However, the viral particles in the brain tissue are not next to where there is injury or damage," she says.
Frontera suspects that's because the virus is a "bystander" that doesn't have much effect on brain cells. But other scientists say the virus may be cleared from brain areas after it has caused lasting damage.
Researchers agree that, regardless of the mechanism, COVID-19 presents a serious threat to the brain.
Frontera was part of a team that studied levels of toxic substances associated with Alzheimer's and other brain diseases in older COVID-19 patients who were hospitalized.
"The levels were really high, higher than what we see in patients that have Alzheimer's disease," Frontera says, "indicating a very severe level of brain injury that's happening at that time."
It's not clear how long the levels remain high, Frontera says. But she, like many researchers, is concerned that COVID-19 may be causing brain injuries that increase the risk of developing Alzheimer's later in life.
Even COVID-19 patients who experience severe neurological problems tend to improve over time, Frontera says, citing unpublished research that measured mental function six and 12 months after a hospital stay.
"Patients did have improvement in their cognitive scores, which is really encouraging," she says.
But half of the patients in one study still weren't back to normal after a year. So scientists need to "speed up our processes to offer some kind of therapeutics for these people," Frontera says.
Also, it's probably important to "treat that person early in the disease rather than when the disease has advanced so much that it has created damage that cannot be reversed," Serrano says.
All of the researchers mentioned that the best way to prevent COVID-related brain damage is to get vaccinated.