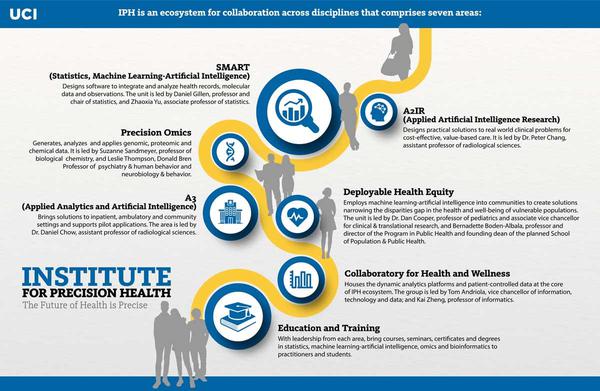
The Institute for Precision Health (IPH) at the University of California, Irvine (UCI) is an ambitious effort combining the university’s various capabilities directed at precision medicine progress. According to representatives, the IPH’s work will aim at delivering effective health and wellness solutions for each patient, thereby addressing problems with health equity and high care cost.
To find out more about the UCI’s mission and its efforts to come up with advanced solutions in precision medicine, Outsourcing-Pharma connected with a number of university leaders:
OSP: Could you please share an overview of some of the key developments/advancements in precision health in recent years?
SS: Physicians have known for years that individuals differ in how they respond to therapies. The idea of precision medicine is that individualized care could be delivered at scale. Although this has not yet been fully realized, the promise remains, the progress that has occurred has allowed us to more clearly focus on the challenges that remain, and much has been accomplished.
Emphasis on genomics has supported large-scale genome sequencing projects across many ethnic groups that for the first time is enabling identification of genes that affect the health of individuals in many different ways. Collection of information on this is allowing insights into genetic changes that affect behavior and health. These population-scale studies include the UK 100,000 Genomes Project, US Million Vets, and All of Us projects, in addition to other studies.
This information has changed the face of medical care:
LT: Ability to use a variety of data types – e.g. medical information and genomics – to more clearly understand human diseases such as Alzheimer’s and cancer. It is truly becoming a reality that we can develop diagnoses and therapies on an individual basis. For instance, we are understanding subtypes of patients with Amyotrophic Lateral Sclerosis by carrying out multiple types of genomics including sequencing patient DNA and integrating it with their clinical symptoms.
OSP: Please tell us about some of the notable precision medicine programs and projects at UCI in recent years.
SS: Data-sharing collaborator: Under the direction of Kai Zheng, this is one of the most notable precision medicine programs at UCI. Under this program, EHR data can be made available to researchers in formats compatible with study design or directly mining data. Previously this was not possible, in the last months there have been multiple outreach seminars covering access to All of Us genomic data, to records related to COVID patients, and other studies.
COVID host project: It is known that children can be virtually asymptomatic in response to COVID or can suffer from acute inflammation. In this project, representing an extension of an adult host sequencing project conducted among the UC’s, UCI collaborated with CHOC to consent young patients for samples to be used for germline wgs. This project has passed the first stage with support from PHAI for the consenting and collection of samples at CHOC and wgs which was conducted at UCI GHTF.
To date, 27 genomes have been sequenced and it is anticipated that assembly and analysis of the 27 genomes will be completed by the end of May 2022. Analysis of the genomes for variants that appear associated with more severe disease will then be funded under the PHI Precision Omics umbrella.
Identification of unknown neuromuscular disorder: Pompe disease is a rare, typically heritable lysosomal disease usually caused by defects in alpha-glucosidase causing muscular weakness. Tahseen Mozaffar MD Ph.D. is a UCI expert in this disorder.
As part of a Pompe study, in collaboration with an investigator at UCLA, it was determined that about 500 patients had the symptoms but not the mutations that characterize Pompe disease. Of these 96 were distinguished by having elevated creatine kinase, an enzyme found in heart, brain, and skeletal muscle. Elevated levels are associated with muscle damage and late-onset Pompe disease. However, this subset of patients does not have the typical mutation spectrum of Pompe.
The PHI study is designed to investigate the basis of this non-Pompe genetic disorder. Two genomic approaches are being taken. This study will be the first to use the Illumina beadarray iScan instrument to survey 2 M single nucleotide polymorphisms (SNPs) across the genome of each of these patients. In addition, exomes, encoding the proteins in these individuals will be examined by targeted sequencing. If mutations exist in coding regions that might directly negatively affect protein functions, these can be identified.
These approaches are synergistic. If mutations are identified in the exome sequencing, inferences regarding the SNP mapping data to nearby non-coding sequences may be empowered.
The Precision Omics unit: This is a research-based facility for the development and application of genomics tools to empower biological insights. This unit makes available to UCI investigators a range of genomics technologies including optical mapping for detection of chromosomal rearrangements, whole-genome sequencing for identification of genetic variation, measurement of gene expression, and measurement of epigenetic changes that may reflect changes that may be perpetuated over multiple cellular generations.
Current investigations include understanding genetic and gene expression changes and cellular interactions in colon cancer, gene expression in muscular dystrophies, cellular changes in melanoma, and wound repair. The most exciting area of research development has to do with measuring gene expression in single cells and most recently mapping those gene expression patterns spatially in the tissue.
Multi-omics is an area of development in which multiple technologies come together to produce a better understanding of tissue dynamics. For example, by combining technologies that elucidate chromatin structure measurement and gene expression (ATAC-seq) or by combining protein measurements and changes in DNA to allow mapping of tumor development and metastasis with molecular precision.
LT: The Vulnerability Scoring System (VSS) is used to understand what COVID patients would need most intensive care in the hospital. Carrying out DNA sequencing of hospitalized COVID patients as part of a UC-wide effort to understand the genes that might make an individual more susceptible to severe COVID versus less severe. Using genomic information, identifying a drug that may reduce COVID viral infection (in development). Carrying out genomics on pediatric patients with unknown causes of muscle weakness disorder to discover the genes involved. Genomics to inform cancer treatment of individual patient subgroups.
OSP: Please describe the Institute for Precision Health in a nutshell. Please talk about how you decided to launch the institute, the key players, and some of the notable features of the program.
TA: The ever-evolving capabilities of the IPH herald a future of tailored care that alters the healthcare landscape to place the patient at the center and in control. In the past, individuals were treated based on approaches thought to be best for groups of patients. Now, we begin the epoch of patient-centric care designed to continuously improve the health of the individual within their community, even as new knowledge accrues, whereby rights, incentives, transparency, and control remain the purview of the patient. Advances are scalable and open-source, so they improve healthcare and wellness in California, the nation, and around the globe. Success will be measured as improved patient outcomes, cost-effectiveness, and equity.
LT: Bold and innovative initiative to leverage expertise across UCI and with industry partners to use the newest approaches and strategies in artificial intelligence and machine learning, combined with advanced genomics and a novel platform that can house multiple types of data to significantly advance the health of our communities. A major aspect and competency of IPH is health equity across populations in Orange County and beyond – bring in the community and the patient as partners in the health mission.
OSP: Please share some detail about the SMART unit—the areas of specialty in the unit, any short- or long-term goals, what Drs. Gillen and Yu will be tackling.
DG, ZY: The Statistics, ML, and AI Research Technologies (SMART) unit is focused on developing statistics and ML/AI methodological solutions and data science techniques to address foundational challenges and unique problems posed by various scientific goals of IPH. The SMART unit is led by two faculty of the Department of Statistics - Daniel Gillen and Zhaoxia Yu, who have produced multiple methodologies to leverage the field of precision health. Its overarching goal is to accelerate the discovery of patient-specific treatments and care through innovative research to maximize efficiency, propel discovery, increase generalizability and reproducibility, and validate novel biomedical interventions.
The four primary components of SMART are to develop innovative data ascertainment methods and procedures for maximizing information from HER data, to develop novel prediction and discovery methods, to develop rigorous methods for common problems in the integration of observational and HER-derived data, and to assess and validate statistical methods for efficient and adaptive designs of clinical studies.
While SMART will focus on the foundational elements of statistical and ML/AI methodologic development as motivated by scientific goals of PHI, the faculty of SMART has been and will continue collaborating in a synergistic fashion with all other themes of the Institute.
OSP: Then, please share some detail about the A2IR unit, and Dr. Chang’s work
PC: The Applied AI Research (AIR) unit is comprised of a seasoned data science team with expertise in using state-of-the-art machine learning methods to solve healthcare challenges. The unit is led by me, a physician and full-stack developer with over a decade of experience building FDA-cleared software tools in both the academic and commercial setting.
The AIR team translates foundational ML methods developed by the SMART unit as well as industry leaders into AI-enabled software applications validated by the A3 unit, together in close collaboration with domain experts and resources of the remaining IPH units.
As a central data science hub, the AIR team has over a dozen active projects across the UCI community, with current focuses in cancer (brain, breast, gastric, renal, and prostate), stroke, and infectious diseases. The AIR team comprises faculty, data scientists, graduate students, and trainees from UCI, the Children's Hospital of Orange County (CHOC) and the VA Long Beach Healthcare system.
OSP: Similarly, please tell us about the A3 unit.
DC: A3 (Advanced Analytics and Artificial Intelligence)’s goals are simple - we seek to improve care by focusing on operationalizing A3-driven solutions that improve clinical workflows, efficiencies, and ultimately care delivery. And to point out, some of these solutions may be homegrown through initiatives like AI2R or procured through strategic investments.
That sounds very buzzy partly because there is no universally accepted definition of digital health. Broadly, I think digital health takes data to improve health. While there are numerous ways to go about this, our group focuses on solutions that center around tools that leverage advanced analytics and artificial intelligence.
Our approach is also simple. I mentioned the environment in my opening line, which is at the heart of our operating model. It allows us to focus on many different challenges in parallel, which allows for faster usage.
What’s exciting about this model inherently continually improves and really focuses on learning and becoming more adept in not only identifying issues but ultimately predicting issues before they happen. For example, our COVID risk calculator did not start as a prediction tool. We initially focused on data quality of our COVID-19 patients.
Working with our clinical teams, we identified discrepancies in lab ordering habits given the novel disease. As a result, our hospital within two weeks' start was able to create a standardized lab panel, yielding better data.
Having improved data, and expertise from public health, we soon identified that there were specific at-risk populations in Orange County, CA. Moreover, we were able to begin to develop a tool that could stratify high risk from low-risk patients. Within three months of the COVID-19 pandemic hitting UCI, we were able to translate these efforts into a risk prediction tool for our clinicians.
In parallel during the pandemic, we were able to support an initiative to improve stroke care delivery. We have since brought down our notification times for a stroke from above 30 minutes to under 5 minutes, even amongst our trainees! But it doesn’t end there. It’s now focusing on how this improved time savings can improve care.
These are just a handful of examples. Moving forward, we are looking at projects within spine surgery, sepsis, etc. to name a few.
OSP: How about the Collaboratory for Health and Wellness unit?
TA: The Collaboratory for Health & Wellness is our data analytics platform, but the Collaboratory also represents a process for how we bring together diverse data from across the health spectrum and contextualize it to make data an engine for insight, collaboration, and impact.
The Collaboratory is boundaryless in its design to span distance, support rich recurring interaction, foster interdisciplinary discovery, and provide access to data specifically curated for a problem statement. Today’s healthcare challenges require not just data and deep subject matter expertise but also should embrace a mindset around open source, inclusivity, ecosystem thinking, and health consumer enablement. Our Collaboratory concept, which we use across UCI, is our demonstration of this approach.
OSP: Could you please tell us about the Precision Omics unit, and the work of the professors there?
LT: We have extensive expertise and state-of-the-art equipment to discover and implement the tools of genomics that will create a molecular “blueprint” or “snapshot” of each patient. These are becoming higher-throughput and will be integrated with health data. An advantage of being within IPH is the ability to use advanced computational methods and analytics to integrate all the data types together and rapidly optimize health care delivery.
OSP: How does Deployable Health Equity come into precision health? Please talk about why this is important.
D. Cooper: The COVID-19 pandemic served as a crucible in highlighting the essential role of health data in identifying and addressing critical issues of health disparities and inequities. The interplay of social determinants of health (e.g., income, crowding, access to food, etc.) and a novel virus revealed that the initial burden of the disease was profoundly unequally dispersed across our population.
IPH is determined to build AI and ML tools and approaches to health data so that early signs of disease and health disparity can be addressed before such disparities become intractable and generational. Modern data science can coalesce health data with a myriad of determinants, ranging from air pollution to greenspaces.
The IPH team of clinicians and scientists can then use these often nonintuitive interactions to rapidly deploy health resources. This approach can bolster the effectiveness of a variety of movements currently underway that are focused specifically on eliminating health disparities.
School-based health centers, for example, are recognized as one of the most cost-effective and beneficial health-delivery systems that have a large and lifelong impact on eliminating disparities in minority communities. Novel use of wearable health monitoring can begin to address other emerging issues of health disparities such as the rising rate of antenatal pregnancy complications among African American women or increasing rates of certain lymphomas in our Latino population. IPH will work to access currently available data, such as state-mandated, school-based physical fitness data, to identify trouble spots of childhood obesity and physical inactivity, and work with regional organizations to implement and monitor solutions.
In sum, IPH embraces the unique challenge of using data science and precision health to identify health disparities and monitor and evaluate efforts to mitigate them.
OSP: Is there anything else you would like to tell us about the Institute?
TA: In our view, IPH represents the potential future for health and healthcare. In a time when the intersection of science and technology is pushing the boundaries of understanding health and disease, UCI realized a multidisciplinary institute was required to tackle the complex challenges ahead and the opportunity to enlist all parts of our research university in addressing those challenges. The pieces brought together represent both the opportunities and risks associated with a data-powered healthcare future.
Our deepening understanding will allow us to understand disease and its progression at levels never before seen and at the same time allow us to personalize our treatment pathways for each patient. Additionally, we feel with all this potential comes tremendous responsibility for transparency and equity. Some of the same capabilities, if not taken in a thoughtful manner, can lead to greater disparities and access to high-quality health care, and improved patient outcomes.
Our thoughtfulness about the necessary components for IPH represents the imperative to address from the beginning stages of exploration issues around design and deployment aspects that can ensure equity in the leveraging of new technologies and data-driven approaches.
LT: A goal is to provide a global perspective on health and create a multidisciplinary hub across UCI that can benefit researchers, clinicians, and the community to advance health equity and effective treatments. IPH will fundamentally facilitate the academic health mission of translating findings to the clinic and training the next generation of experienced researchers in precision health.