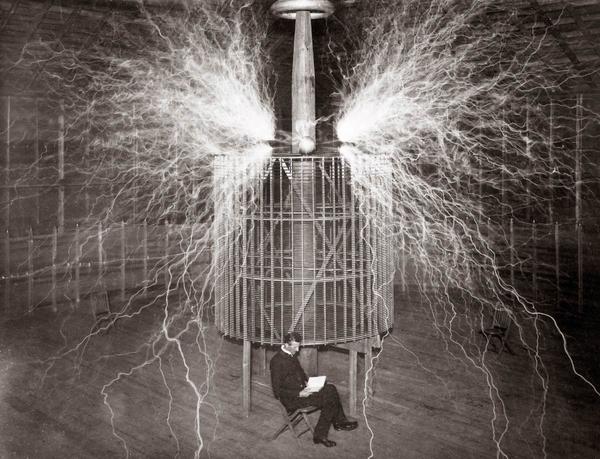
The electric engine, invented in 1834, was touted as the productivity booster that would revolutionize manufacturing. Yet it took three decades before it had a real impact.
When factories replaced steam engines with electric motors but left in place systems built around the old steam-based drivetrain, electricity offered no new efficiencies. It wasn’t until factories were designed from the ground up, with production lines intentionally built for the electric era, that manufacturers made enormous productivity gains — up to 90% — with the introduction of new production lines.
In health care, the equivalent of replacing the steam engine with the electric motor is removing the stranglehold of the doctor-patient visit.
advertisement
Say you’re a single mom trying to manage your diabetes. For you, conventional health care is both sporadic and time consuming. Going to see your doctor often means taking time off from work; paying for parking or public transportation or an Uber; waiting; undergoing a battery of tests that provide a single snapshot of your condition; and waiting some more. The grand finale is a short conversation with your overworked doctor who has little time to discuss everything you’ve encountered since your last visit.
For the “privilege” of this doctor-patient visit, you may face substantial out-of-pocket costs if you have a high deductible.
advertisement
Now reimagine the scenario based on technology that’s already here: After your initial diagnosis, your provider could monitor your blood sugar remotely. If a pre-programmed tool detected an increase, it would ping a member of the care team who could give you a call or start a text discussion to find out how you’re doing without needing to bring you into the clinic. A nurse could troubleshoot whether you’re taking your medication, call in a refill if needed, and discuss options for how you can pay for it. If you needed education about taking your medication, a pharmacist could call and follow up at a time that worked for you. The nurse could also ask you about things like stress and diet, and make recommendations for online resources or referrals to in-network nutritionists.
If your blood sugar did not come back under control, only then would you need to make the trek for an in-person doctor-patient visit.
Making way for digital innovation

Allowing the synchronous doctor-patient visit to maintain its stranglehold on health care means missing huge opportunities for digital innovation. The health care system must make the most of the new technologies that allow clinicians to communicate with their patients on patients’ terms, meeting them where they are. That means making the most of new data sources that can be captured passively using sensors that measure motion or breathing rate or blood sugar and leveraging the power of modern computing to analyze and gain insights into patients’ unique experiences.
Using the full range of communication and digital health technologies available today, care can be built around the patient, not the clinic. Breaking the focus on the in-person visit means being able to measure health care by how little people actually need and how healthy they can stay, not by how much health care is consumed or even how good clinicians are at helping heal the sick. Reengineering clinical workflows and systems of care can get the best out of every member of the care team, minimizing how much time patients must spend in doctors’ offices while ensuring they receive the best possible care.
The pandemic has added extra urgency to solving the issue of time spent in doctors’ offices. Covid-19 has led to overfilled emergency rooms and overstretched doctors, and demonstrated that a more data-driven, fit-for-purpose approach could improve the lives of patients and the clinicians who care for them. As the pandemic continues to rage, now is the time to use these tools and learnings to make a more permanent commitment to managing patients’ health and the health of the clinical workforce more holistically.
Manufacturing had to wait decades to be transformed by the electric engine because the impact of this innovation was blunted by sticking with existing systems. Health care doesn’t have that kind of time. Under the long shadow of the pandemic, there’s an immediate urgency to build care around patients, not clinics. This requires a move to continuous, team-based models of care that leverage technology alongside appropriate clinical and non-clinical professionals to address the crises of quality, safety, access, and equity.
Innovative providers are leading this transformation, capturing soaring digital health investment dollars to build care delivery systems anew in the digital era. But while leading innovators will put pressure on the traditional system to evolve, fundamental change will require new payment incentives that match this approach to care delivery and recognition of value in new approaches to care delivered beyond the confines of clinic-based visits.
Health care is at a breaking point that could leave behind the people who need it most and further disenfranchise the clinicians who have borne the brunt of this crisis. The scourge of the pandemic has not only rendered an opportunity to act but a shared responsibility to create new, sustainable structures that allow both the patients the system exists to serve and the professionals it depends on to function to live healthier lives.
Jennifer Goldsack is the CEO of the Digital Medicine Society. Soujanya (Chinni) Pulluru is a family medicine physician and senior director of clinical transformation for Walmart Health and Wellness.